An infectious disease is classified as a pandemic when it is widespread across multiple countries. There is also usually a requirement that it have a certain degree of severity. There are many cold viruses that are worldwide, but are not normally considered pandemic because their symptoms are mild.
The H1N1 flu, or "swine flu" because it came from pigs, was declared a pandemic in early 2009, and it lasted for about a year and a half. At the time, epidemiologists were worried about this particular flu because the last time a flu virus classified as H1N1 spread worldwide was 1918. Here is a graph of life expectancy in the US. Note that neither WWI or WWII killed enough Americans to make a noticeable blip in the graph. But because that H1N1 strain killed large numbers of young adults who would normally live many more years, it is really obvious in the graph.
 |
| US Life Expectancy |
So when a new variety of H1N1 started to spread rapidly, more rapidly than normal seasonal flu, epidemiologists took notice. The virus also disproportionately affected young people, just like in 1918. Because it was a flu, though, we already had structures in place to put a vaccine into production quickly. The US has huge flocks of chickens in undisclosed locations that lay eggs that we can grow the virus in to make flu vaccine. So the flu vaccine machine swung into action, and there were lots of news reports telling people to be sure to get their flu shot that year. I remember getting mine.
There were some localized quarantines and school closures, especially early on, but it eventually became apparent that even though the virus was spreading rapidly, it was not like the 1918 version in terms of disease severity. It was actually less fatal than the regular seasonal flu. In the end, the case fatality rate was 0.03%, compared to about 2% for the 1918 flu. Those most at risk of death from the 2009 flu were young children and pregnant women (pregnancy suppresses the immune system). So even though it infected somewhere in the neighborhood of 15% of the world's population, deaths were probably less than half a million worldwide. By comparison, the 1918 flu infected about a quarter of the world's population, and killed somewhere between 1 and 6 percent of all people alive at the time.
The vaccine probably helped. We know that it's not hugely effective, but it's better than nothing. Even if your immune system didn't get activated enough to create full immunity, it might be enough to reduce disease severity.
Now if we look at the current pandemic, we have a coronavirus instead of a flu virus. We have never successfully created a human coronavirus vaccine, so we don't know if it's even possible to do so. We know that there are four human coronaviruses that cause mild symptoms, and two human coronaviruses (SARS and MERS) that are horrible. SARS has a 10% fatality rate, and MERS has a 34% fatality rate. So right from the beginning, the CDC and WHO were watching what was going on in China with this new virus.
The new coronavirus is officially called SARS 2, which I think is rather confusing, so I'm going with "new coronavirus" or "this virus," or "covid-19 virus." Covid-19 is the name of the disease, rather like AIDS is a disease caused by HIV.
The fatality rate of the this new coronavirus is not as bad as SARS or MERS (thank goodness!). It's fatality is far worse than the H1N1 flu virus, though. It may be in the neighborhood of the 1918 flu that everyone was afraid of in 2009. I have another post about trying to understand the case fatality rate
here, and I concluded that it might be in the neighborhood of 2%, which is roughly what it was for the 1918 flu.
The insidious thing about this virus, compared to SARS and MERS, is that about half of the people, even older people, who get it have no symptoms. So they spread it without even knowing. With SARS, we were taking temperatures at airports, and if you had a fever, you couldn't get on the plane. MERS made people so sick that they couldn't spread it if they wanted to. So those diseases were relatively easy to control.
This new virus has an unusually wide spread of responses from different people infected. Half have no symptoms, but roughly 20% get very ill and need medical attention, and 1-2% die. There is a lot of concern that if 20% of the world's population gets it, and 20% of those need medical attention, that means 4% of all humans are going to need the attention of the medical system. Because it's spreading so quickly, all those people are going to need medical help at about the same time. That's going to overwhelm the medical system. The medical professionals are gearing up for things to get much worse, but there's only so much they can do.
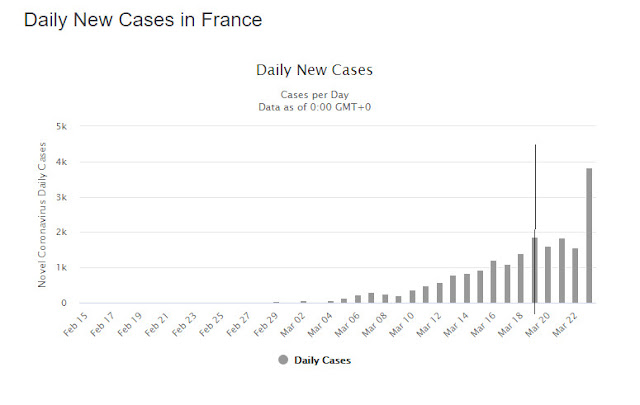
The covid-19 virus is spreading rapidly, probably more rapidly than the 1918 flu. Numbers have come down in China and South Korea, but all of Europe and the US are still on the rise, both in terms of cases and of deaths.
We don't know yet how much it will spread. That depends on so many factors, like social distancing and whether or not we can come up with a vaccine. It will probably not be as bad as the 1918 flu, but it's already worse than the 2009 flu.
It isn't the end of the world. The human race has survived far worse bouts of infectious disease. But it is a reminder that we are more vulnerable than we think we are.